September 6, 2018
The federal government is deciding how to proceed on national pharmacare. Whatever path it chooses, federal action on pharmacare will need to carefully consider its interactions with an existing landscape of provincial programs. Failure to do so will result in Canadians being treated differently based on province of residence, an outcome certain to spark resistance from provinces whose residents are unfairly disadvantaged.
All of these approaches will be more expensive to implement than a simple exercise of filling existing gaps in pharmacare coverage. But this will be essential to getting provinces on board.
Here are our key takeaways:
-
All Canadian provinces already have some form of public pharmacare coverage
Typically, this coverage is some mix of three models – “catastrophic” coverage of high-cost conditions, needs-based coverage of specific populations such as seniors or low-income residents, and public insurance for individuals not covered by private plans.
As a result, any national pharmacare program would not be entering an empty field but an area already packed with long-standing and well-entrenched provincial initiatives.
-
Any federal action will necessarily interact with the dozens of provincial programs
Though all provinces offer some form of coverage, they differ widely in terms of the mix of models they employ and the requirements for enrollment in specific programs. In addition, existing federal pharmacare programs cover specific populations such as First Nations and Inuit or refugee claimants. Between 61 and 76 per cent of each province’s population also have private insurance. Many Canadians also still pay for medication out of pocket.
Any successful federal pharmacare initiative will need to work out in detail how the national program will interact with the existing landscape of drug coverage.
-
The existing pharmacare landscape leaves a host of policy problems and gaps unaddressed, which the federal program will need to consider
Currently, Canadians have different coverage based on their province of residence. Some Canadians are not eligible for coverage at all, and many more do not enroll in the coverage they are eligible for. Other gaps that remain unaddressed include issues of affordability or inconsistency across program parameters and formularies. Canadians also pay higher prices for drugs and rely more on private insurers than many other western countries.
Identifying and resolving these policy issues and gaps will represent a significant challenge for any national pharmacare initiative.
Any federal action on pharmacare will need to carefully consider its interactions with an existing landscape of provincial programs.
-
Each model addresses some problems and gaps better than others, meaning that the national program will have to make tough choices
A national pharmacare program could take a number of different forms: coverage for catastrophic drug costs, mandatory coverage, targeted filling of gaps left by existing coverage, and universal coverage. Whatever model the federal government chooses for the national pharmacare program, the program will be able to address some, but not all, issues and gaps that exist in the current provincial pharmacare systems. The federal government must therefore choose among, and trade off, important policy goals, including cost.
-
Each model, applied nationally, will raise cross-provincial equity issues that could severely complicate any federal action on this issue if interactions with provincial programs are not considered
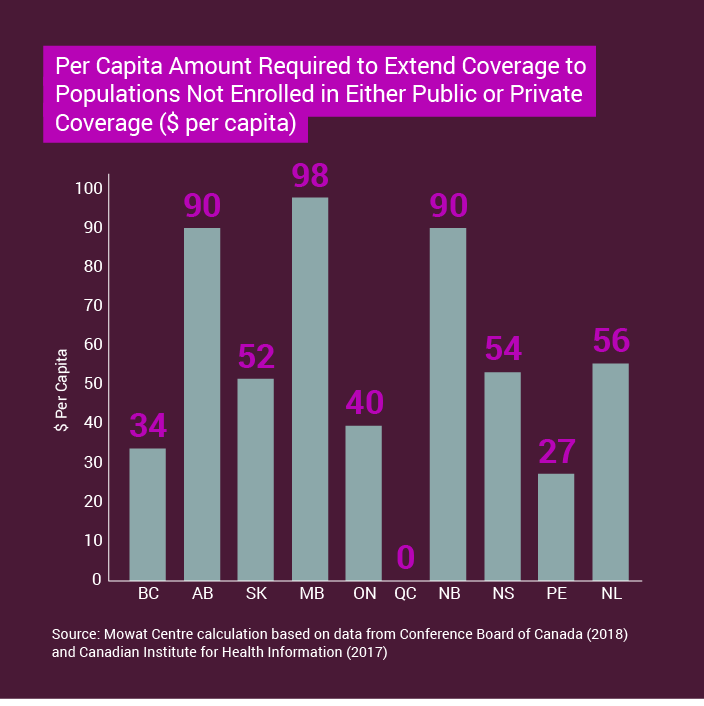
A key feature of the existing pharmacare landscape is that Canadians differ in their current pharmacare coverage based on their province of residence. Any national program would, if simply layered on top of the existing pharmacare policy patchwork, result in the residents of some provinces getting more from the federal program than others.
This presents a potential minefield for the federal government that, if unaddressed, could derail whatever approach it chooses to take on pharmacare.
-
Established principles and approaches of fiscal federalism can help the federal government successfully navigate this intergovernmental terrain
Canada’s system of fiscal federalism has a number of established principles and approaches that should guide federal-provincial interactions in Canada. These include horizontal equity, maximizing comparative advantages, risk-sharing, asymmetrical federalism, and others. These principles and approaches should be used to guide governments towards legitimate, equitable and fair arrangements that achieve policy goals while navigating through intergovernmental obstacles.
In practice, these principles are often traded off against each other as well as against a program’s cost. The case of national pharmacare will be no different. In a number of likely scenarios, adhering to established principles and approaches of fiscal federalism will increase the cost of the national pharmacare program. But departing from these principles and approaches risks failing to achieve a national pharmacare program that delivers positive impact for all Canadians.
-
Whichever objectives the federal government chooses to prioritize with a national program, there are pre-existing fiscal federalism approaches well-suited to achieving them
Our analysis shows that each model can be accompanied by an appropriate use of the established principles and approaches of fiscal federalism. Should the federal government choose to implement a catastrophic coverage model, this choice would be best served by the use of federal spending power to replace provincial programs. A mandatory coverage model and a gap-filling model would be best served by the federal government setting and fully funding national standards that apply in all provinces. A universal coverage approach would be best served by direct payments from the federal government to individual Canadians, similar to other federal transfers to individuals such as Old Age Security or the Canada Child Benefit. The expense of a universal coverage approach could be defrayed by reduced federal health transfers as compensation for the federal government’s assumption of a greater degree of fiscal risk.