February 22, 2017
Universal health care in Canada is strongly attached to Canadian values such as equity, fairness and solidarity. It is also, however, a mechanism for sharing risk between citizens. When we see ourselves as equally vulnerable to the random but potentially catastrophic impacts of illness, the value of sharing the costs of insuring against it becomes apparent. In Canada, we have operationalized this risk-sharing system through publicly-funded and universally-available health care.
Entanglement, however, necessitates collaboration.
The collaborative approach Canada’s orders of government initially took in establishing universal health care required cost-sharing to make it work. Running an open-ended citizen demand-driven program comes with significant fiscal risks. The federal government occupied a greater share of the tax room in Canada at the time (and still does). So cost-sharing was seen as fair way of balancing the federal government’s spending power with the provinces’ jurisdictional responsibility for health care.
While financing arrangements and scope of health programming evolved somewhat after the initial era of explicit cost-sharing, the block funding arrangements that replaced them in 1977 still sought to share costs. Not on a perfectly equal basis, but close. It wasn’t until the federal budget cuts of the 1980s and 1990s that the federal government began eroding its financial support for health care, consequently transferring significant fiscal risk to the provinces. Revenue raised by provinces now funds over three-quarters of health care spending.
Looking forward, the federal government’s current approach to negotiating a new health accord appears poised to repeat the mistakes of the 80s and 90s by continuing to erode its level of support for health care.
In its election platform, the current federal government committed to negotiating a long-term health funding arrangement with the provinces. Its chief negotiating tactic on this file thus far, however, has been “take-it-or-leave-it.” While the Atlantic Provinces, Saskatchewan and the Territories have taken the offer – with “me too” clauses to ensure that if someone else negotiates better terms, they get the same deal – 90 per cent of Canada’s population is still uncovered by the new health accord.
The main issue for the provinces who have “left it” is that the federal offer is inadequate, and leaves the provinces exposed to the majority of the fiscal risk that comes with running the health care system.
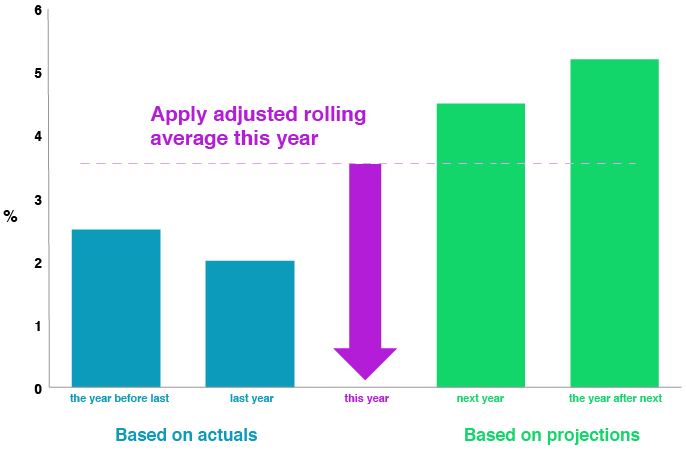
The offer extended to provinces in December was to continue the “existing legislated commitments through the Canada Health Transfer (CHT).” Apart from small incremental investments in home care and mental health, that is what was going to happen anyway. According to the framework laid by the previous federal government, the CHT will grow at the rate of a three-year moving average of GDP growth. The evidence suggests that this rate of growth – estimated by the Institute of Fiscal Studies and Democracy to average 3.7 per cent over the next decade – will not keep up with the projected rate of growth in heath care.
In December provinces argued that, rather, a 5.2 per cent growth rate in the CHT will be necessary to meet the actual cost pressures provinces will face over the next decade. A recent report from Ontario’s Financial Accountability Officer gives credence to that argument, estimating that health sector cost drivers will lead to expense pressures of 5.3 per cent per year to 2020. Beyond that point, provincial health care systems are projected to groan under the weight of an aging population. The first of the baby-boomers (born in 1946) turned 70 this year. In ten years, they will turn 80. Seniors account for a larger per-capita share of the health budget, so as the large cohort of baby-boomers ages, they will represent a growing strain on provincial health budgets.
While pegging the growth rate of the CHT to GDP and then walking away for a decade may be appealing from the standpoint of the federal government, it does not meet the bar of sharing the risk of delivering health care. It is doubtful that Canadians will be content with the provinces being left essentially on their own to deal with the impending demographic challenges to the health care system. The result will be fiscally unsustainable provinces.
Sharing the fiscal risk of health care between the orders of government will produce better results.
The best way to accomplish that would be for the federal government to re-establish its role as a full partner in the health care system. For the federal government to fund health care like a partnership between equals, it would have to add $10 billion to the envelope it currently spends annually. However, in addition to its health accord offer, the federal government has sent some very strong signals that incremental investment of this size is not in the offing.
Sharing the fiscal risk of health care between the orders of government will produce better results.
It appears that the best that can be hoped for then is agreement on a CHT escalator that does not widen the gap between the costs of delivering health care and the federal government’s current level of support.
A modest solution would be to tie growth in the CHT to growth in health care. To be reflective of conditions on the ground, however, the mechanism for setting the escalator should be more flexible and responsive than simply setting it at a set growth rate of 5.2 per cent for a decade.
So how might this be accomplished?
Basing the escalator on actual observed increases in provincial health spending would be one way of doing it. But, lagging the data too much would sacrifice responsiveness in a situation that arguably demands it. Under such a system, it would not take long for growth rates in health and transfers to become misaligned without a built-in way of addressing the gap.
Conversely, an escalator could be based on projections of health spending. But those projections would have to be reliable, and would have to be adjusted if they proved not to be reliable.
A hybrid solution would incorporate the benefits of flexibility and responsiveness while allowing for corrections to ensure reality is not replaced with projections. An escalator based on an adjusted rolling average of projections and actual data would represent such a solution. For example (see illustration below), the escalator for this year could incorporate data for projected increases in health spending for next year and the year after next, as well as actual spending data for last year and the year before last. If projections prove to be either too high or too low, the average could be adjusted to compensate for those differences.
A Model for Using Projected and Actual Health Spending Data to Inform the Development of an Escalator for the Canada Health Transfer
The question remains: who could be relied upon to make the projections of health spending? Both the federal government and the province would have fiscal incentives to make the projections either too high or too low.
The answer instead lies in effective, transparent institutions. Canada lacks a truly pan-Canadian (not federal) institution mandated to promote transparency and accountability in health care. It has been argued that such an institution should report on how wisely health care dollars are being spent by providing evidence-based assessments and recommendations. In addition, it could be relied upon to advise on appropriate projections to inform decisions on growth rates for the CHT escalator. While the federal government could ignore that advice, it would be expected to justify why it is doing so and outline what the consequences would be in terms of the level of support for health care.
It may be argued by some that tying growth in health transfers to growth in health spending would create a moral hazard, leading provinces to unaccountably increase health spending. However, provinces currently fund over three-quarters of health care spending from their own coffers. They have all the incentive in the world to manage costs. Pegging growth in transfers to growth in health care only leaves the federal share of health spending where it currently is.
For now, however, a system that attempts to attach the growth in federal support for health care to what provinces actually spend might be the best that can be hoped for in terms of sharing the fiscal risks of delivering health care. While focusing solely on a CHT escalator will not solve the problem of an eroded intergovernmental partnership in health care, the right escalator can stop it from eroding further.
More related to this topic
Author
Erich Hartmann
Release Date
Feb 22, 2017







